I regularly talk with friends about food. Often over food. I like food. I like cooking. And as a result tend to use as unprocessed-as-possible ingredients, and start most things from scratch.
I have friends who can’t cook, or won’t cook, and I have friends who like the paleo direction, as I do. There is no right answer. But I do think that whatever we use to prepare our meals, we need to be aware of how it is packaged and marketed, in making our choices.
Some labels have more meaning than others. Fairtrade. Farm fresh. Or Red Tractor. Labels which look and sound good aren’t always exactly what they say on the tin, or what we think they mean. Or they mean different things in different countries. Like ‘Bio’ often conflated with organic.
Why do we need these packaging terms at all? Are they all genuine, of substance and meaningful for consumers, or are they marketing ploys?
I think often, on closer inspection, we may find these marketing labels are used to segment the market and make those who can, pay more for ‘better quality’ and ‘choice’ . It does not necessarily mean there is much substantive difference behind the label.
Consumers should in theory drive the market by buying what we want. But do we know what we want or are we led by marketing?
Are we nudged in the direction of the product the vendors want to sell us though clever marketing?
The total 2013 UK advertising spend reached a new high of nearly £14bn, topping pre-financial crash levels for the first time in six years. Companies must think that is money, worth spending.
How free is our choice?
I would like to think we collectively focus on the core value of what we want as a consumer not just for ourselves but for society. Decent, affordable, production aware, nutrition for all.
However reality is that those who can afford choice, worry whether it is organic or bio, chemical free or free range. Those who cannot afford it, are left with the ‘value’ ranges. It’s never marketed as ‘the cheapest option.’
When I was a teen in school, “Home economics,” classes were compulsory but the content changed to become focused on things we were ‘all’ ‘capable of’ – homemade pizza for example. Now we ask ourselves why are so many of our generation and their kids obese? We seek solutions for weight management. Could we not go back to basics, and fix the root cause – teach all of our kids to cook, and I mean, simple, real, food? Teach us all to understand food labels. Accompanied by a living wage for all, we could both eat more simply and I believe it would make savings in health benefits.
We need our children educated not to fall for marketing without understanding it.
Uninformed, we cannot make informed choice.
Our food and our health and inexorably linked.
When it comes to healthcare, we keep hearing labels, and ‘choice’, and it’s wrapped in plenty of packaging. Patient empowerment. Personalised medicine. Patient centred care. I do wonder if we don’t over-complicate simple things.
Can care be anything else *but* patient centred?
Let me ask the question – could we consider just going back to plain language. Without having to put it through ‘Plain English’ first? Patients need care. From other people. Professionals in whom we trust. Drop the patient-centric, patient-led language.
Let’s just have, as our grandparents used to call it, [1] ‘care’.
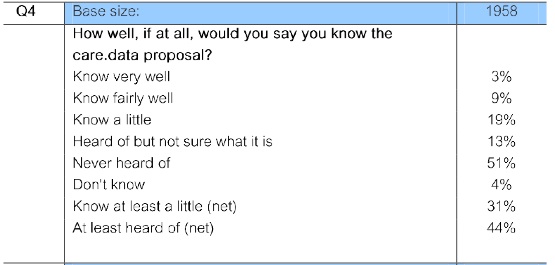
Don’t misunderstand me. I am passionate about patient and citizen participation. It’s why I have spent all my free time of the last ten months understanding care.data and the recent NHS market changes. But it’s the way it is packaged to us, I would like more people to explore and to question whether we really need all the outside layers, or whether it detracts from the most important questions.
Is all the talk around patient-centric really a move towards passing responsibility for payment?
Most people are responsible in their own healthcare as far as they can be. When we can help ourselves, we mainly do. Most people actually are not that good at asking for help, even when they need it. We like to be self-reliant. We know we could eat better, drink less, exercise more. We know we need to manage our treatments and lifestyle. We do, and honestly, if we don’t always do it, it’s not going to help us by repackaging the responsibility, which we know we already have. The majority of people are as responsible as they feel able to be.
Many are pushed to their limits in society of how much more responsibility they can take on. They struggle to feed and care for their families, and don’t ask for help until they really have no other option. We may not want or be able to take on extra responsibility. When we are vulnerable, we trust others to help us.
Choice in those circumstances, is a luxury that’s not high on the priority list. Choice becomes a catchphrase, not a reality. It’s not just that for everyone, but that’s the point. Choice becomes open to some, and closed to others. Some can choose organic, others are left with the ‘value range.’
It’s not perhaps PC to stand up and ask this of everyone with the best of ‘patient-centred’ intentions. I love and commend the intentions here.[2]
I love the spirit that patient leaders intend to ‘enable’ patient empowerment, but what does that really mean?
To me, it infers the belief we patients have no power and therefore no responsibility, right now. It infers we need some seismic shift in current care. I disagree. Care in which I have been involved has always been about a co-operaton between the professional and patient needs, and respectful. It’s what our professionals *do*. It’s already a partnership of trust and we trust professional opinion to take much of the responsibility for our care, in our best interest.
Yes we can get labelled as a bed or a surname. Yes, there is always room for improvement. Some have had awful individual experiences. It is perhaps a luxury of relativley good health that my family has experinced simple and good care, and perhaps it is for those who have more complex conditions that the system must focus improvement.
But are we not in danger of getting so focused away from care and on the patient-power as marketing jargon that we forget that the patients are simply, people, in need of professionals, who care?
We lose focus on asking how is the delivery of that care being supported by those responsible for it, from the top down?
Are we so focused on the solution, and this drive for change, that we are not asking, what is the root cause behind this need?
When we hear farm fresh and bio, we tend to conflate them with healthy, and better for us. If a package says tomatoes, vs bio tomatoes, which do you go for? But just the word ‘bio’ may be a meaningless marketing term. It’s a promotional tool, to make us want it. It is not the same as regulated words which mean not chemically treated, for example.
And so it is with health.
In all this ‘talk’ of patient power, is the real deal deliberately obfuscated?
Being told we should have choice, is to make us want something, demand something, create a demand in patients that in fact, we may not want at all, but start to believe we do.
Is there really a patient desire across so many of us for choosing our own hospitals or do we not just want to go somewhere near, which our families can visit to get good care? Reducing monetary inefficiences is becoming conflated [3] with overall improvement – seeing care only as a supply chain product.
Is there really a need for the drive for ever more comparison data between consultants and between GPs which we are told supports ‘choice’?
Is a market being created, for which there is little public desire?
In a market driven by payment-by-results, fewer patients can mean fewer pounds. GP Boundaries are due to be abolished in October 2014. More GPs are going to be forced to close if nothing changes in funding. Or they amalgamate or are taken over by corporate private management, like this practice. [3b] ‘Choice’ may exacerbate these changes. And it was foreseeable, as Sir Kinglsey Manning predicted in 2006 in the Inevitable Decline of the GP Partnership.
Are we being manipulated into wanting what others want us to want? Is the patient-centric conversation keeping us distracted from the overriding factor in current policy – the drive from top-down to cut costs? The choice made by Government to create a gap between need and what is being provided from the public purse strings?
Between the 2012 Nuffield Report [4] and today’s £30bn, there must be reliable numbers somewhere. As a lay patient, it’s hard to know what is reliable and how to get an informed understanding.
It will be even harder to make a patient choice, if there’s no money available to offer any services to choose from.
If we can’t afford to be self-payers, privately insured, what then? This is the real impact patient choice will have. Some will have choice, and many will have none. Some will have care, and many will have none.
We will have facilities closed, which cannot offer care. And facilities open, where patients cannot afford to go.
Twenty years on, Yes Minister still makes me laugh. It’s possibly even less PC now, than it was then. But are some of the storylines still relevant? Perhaps more than ever.
“Get rid of 300 of your people, and get some doctors, and nurses, and get some patients.” | Yes, Minister – the Compassionate Society
We hear now increasingly of the secondary care closures, and the looming primary care crisis in GP recruitment and we ask, what shall we do?
We need to stand up and demand fixes for the root causes and not pussy foot around with words and the PC solution to an artificial need, which avoids the basic issues. Shortage of cash and staffing.
Patients must better understand the changes in this market creation for it to work – but not all change is equally good
University fees still make studying medicine expensive, even if part supported. GPs are not always, contrary to some media-hype, the best paid in medicine. It is interesting to look at a study in the unit costs of health and social care [5]. When students draw towards the end of their expensive studies it is unsurprising many look for the best paid jobs and specialisms may appeal. I recently spoke with one mid-year student about her future and she was looking at brain surgery or psychology. The reason? She thought GPs in the future of the NHS was ‘too unpredictable’.
The seniority pay system has been scrapped for new entrants and reduced for those already in, so they can’t look forward to natural salary progression with really good benefits later on either.
Top and tail, the profession has been hacked off, in both senses.
Against a backdrop of regular undermining like the ‘maggotgate’ scandalous misrepresentation in the media, top-down imposed changes have been a heavy burden on GPs who continue to put patients first and care for us.
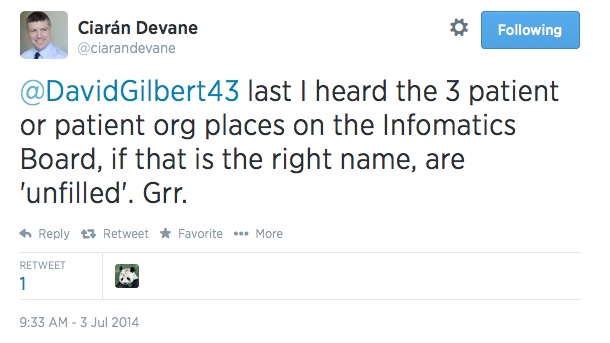
They’re coping with a technical support system [6] under constant tinkering with its admin processes which may not offer any local benefit, changes to core work [7], potential outsourcing [8] and job losses, the destabilisation of support, and both increased marketisation [9] and general lack or stalling of funding since 2010. [10]
And that’s only from an outsider patient’s point-of-view. Patients, ask your GPs.
It feels to me very much as if ministers want to pass the buck (pun intended) back to patients – if we’re responsible for the management of our care today, we’ll likely be responsible for the cost of it tomorrow.
The concept of promoting patient choice, of patient-led decision making though fundamentally not flawed, deflects from the responsibility of others in care provision. It suggests that the patient is to be solely responsible. There are of course aspects of care we can and should manage ourselves. But I don’t feel this is the primary driver of the initiative, in annual reports and roadmaps. It is all about budget, lack of budget and reduced budget.
“Choice” has become the marketing watchword to package the market force of competition to patients.
It has driven wedges between services and broken others apart, causing the lack of integration which is the very thing they now purport to be key to success in health and social care.
A decentralised, and broken up market is easier to manage by private providers, choice for patients exists only by having multiple providers, which only works if you first break up the NHS single delivery model.
We are told that we are to be risk-stratified this year in GP practices, taking our patient records and analysing them at the practice, CCG or Health and Social Care Centre approved site. By segmenting groups who will be most at ‘risk’ and therefore need higher levels of care, they will also assess those who cost the most. These segments focus for example on COPD, Diabetes, Stroke, and the over 75s repeat hospital admissions.
I worry that there are many vulnerable, such as mental health patients, whose segmentation will stigmatise and put them at risk in ever smaller funding pools.
The idea of personal budgets is a slippery first step, to segmenting out treatments and patients who may or may not be covered by NHS care.
An individual budget, a personal shopping basket, can more easily be analysed by a health insurer for example, or simply reduced by the State to be able to buy less at the State till, without topping it up with our own private contribution.
Over 40% of social care users in England [12] are managed in this way. Social care where the issues of AQF have come well documented, as private providers seek ever to reduce costs.
We are rapidly losing control of that social care market. US investors are snapping up the profitable parts of the sector, with the long term prospect of the wealthy self-pay areas provided for by US investors [13], and the poorer local authority-paid homes? well, we’ll wait and see.
Many elderly are left with ‘the cheapest option’. They may or may not think that it is good value.
If patients are empowered as the new consumers in the healthcare market, we need to speak up for what we want
Let’s cut out all the PC talk and talk to government about getting university (medicine) fees reduced or cut. Stop any new reforms and let the profesionals get on with their job of caring. Let’s cut down on the promotional packaging, and management consultant-speak in healthcare. Drop the patient-led, patient-centric. There are pages and pages in brochures on patient empowerment but patients, we need a bit more revolt, questioning why these changes are needed and what is the root of change required. As so wonderfully put recently, we need ‘revolting patients.’ (p.19) [11] We need patients putting first, but let’s first focus on the care.
Care. That’s what matters. It’s that simple. Not patient empowerment, centric or led packaging and labels. Not parcels of personalised care budgets, packaged as ‘gifts’ and choice to us.
We want as patients for our care and the support of the system of our care to be at the centre of focus.
We need the state to manage that there is enough money in the pot to provide a duty of care for all, fairly, and provide enough trained professional staff to do so.
There is a darn big hole predicted of £30bn between planned spend and need. It’s not going to all come from savings from thin air, nor to pay for itself, so patients, who do you think the Government is expecting to pay for it?
Changes have already been made in what is ‘free on the NHS’ i.e. possible to prescribe, such as hearing aids, other areas may be under discussion, for example in kidney dialysis.
Patients, we need not be ’empowered’ to wake up to the marketing ploys. Speak up, or we are complicit in our own downfall.
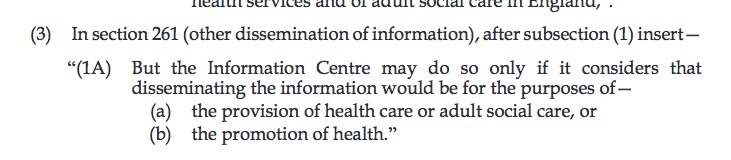
Is this the best path for care in this country, or is it a policy underpinned by an ideology which has removed the Secretary of State’s Duty of Care [14], a duty to provide, and replaced it with a duty to promote?
“The Secretary of State must continue the promotion in England of a comprehensive health service.”
Let’s challenge the drivers of marketing speak and the market based health provision. A market inevitably leads to those who can afford it, having the choice. And those who can’t, are left with the ‘value’ range. They may be left with nothing at all when they need it, if the duty of care, has been replaced with nothing but promotion.
NHS patient empowerment is like buying organic. It’s a false choice. In a system designed to have fair access for all, we should not look to segment the patients, seen as consumers, into those who can pay the most for choice, and those who cannot afford to. Nor should we only see the benefits of personalised budgets.
Let’s ask to talk about the basics. Let’s focus on the care and providing enough funds to do it right. At patient events we need to ask what are the planned costs and where is the budget for them? What is about to be merged with Local Authority budgets for social care? What is ring-fenced and what is not? Where will decision making lie in a merged future?
Where is the Social care and Health Strategy and the benefits plan – have you seen one? I haven’t.
Let patients be patients, and professionals get trained and supported to do their job.
Government, of any colour, must ensure responsibility for the duty of care is not passed along the supply chain. These issues are cross-party and cross parliamentary terms.
The NHS belongs to us all, and should be there, for us all, and not create a three-tiered consumer market in health. Those with choice, those with state care from the ‘value’ range’, and those with neither.
Yes, Minister? [15]
********
[1] Ken Loach made Interviews on the birth of the NHS http://www.thespiritof45.com/Interviews-Archives/Health
[2] Prioritising person-centred care – the evidence http://www.nationalvoices.org.uk/evidence
[3] Wall Street Journal – blog – How Eliminating Inefficiences Can Elevate Hospital Pharmacy As A Strategic Asset http://online.wsj.com/article/PR-CO-20140506-908700.html
[3b] Privatisation behind an Invisibility Cloak – blog by Dr.David Wrigley http://drdavidwrigley.blogspot.co.uk/2014/06/privatisation-behind-invisibility-cloak.html?m=1
[4] the 2012 Nuffield Report- The funding pressures facing the NHS from 2010/11 to 2021/22
[5] Unit Study in Health and Social Care http://www.pssru.ac.uk/project-pages/unit-costs/2013/index.php
[6] Fears for QOF funding as NHS draws up contingency plans to pay GPs from next month http://www.pulsetoday.co.uk/your-practice/practice-topics/qof/fears-for-qof-funding-as-nhs-draws-up-contingency-plans-to-pay-gps-from-next-month/20006085.article
[7] Pulse: Dramatic’ changes to GP contract by next April as Hunt spells out detail of general practice reform, 12 Sept 2013 by Sofia Lind http://www.pulsetoday.co.uk/home/gp-contract-2014/15/dramatic-changes-to-gp-contract-by-next-april-as-hunt-spells-out-detail-of-general-practice-reform/20004293.article
[8] Primary care contracting faces cuts and outsourcing, 5 Nov. 2013 by Dave West – http://www.hsj.co.uk/home/commissioning/primary-care-contracting-faces-cuts-and-possible-outsourcing/5065021.article
[9] NHS shakeup: Private companies see potential to expand their role – Denis Campbell, July 2010 – Firms aim to to gain unprecedented foothold in healthcare system once GPs start spending £80bn of NHS funds – http://www.theguardian.com/society/2010/jul/12/nhs-private-companies-gps-funds
[10] GP Online – Cuts to enhanced services across England will wipe out slim uplifts to GP contract funding agreed for 2011/12, a GP investigation reveals. By Stephen Robinson on the 19 October 2011 www.gponline.com/exclusive-practices-face-28000-service-cuts/article/1099085
[11] Reflections – Have we empowered patients Essay: p.19 Jeremy Taylor, Chief Executive, National Voices
[12] A report by the All Party Parliamentary Groups on Global Health; HIV/AIDs; Population, Development and Reproductive Health; Global Tuberculosis; and Patient and Public Involvement in Health and Social Care – May 2014 – http://www.patientsorganizations.org/attach.pl/1786/2114/APPG%20Global%20Patient%20Empowerment%20Report.pdf
[13] Social Care – US investors snap up UK care homes, FT, June 10, 2014 – by Gill Plimmer – http://www.ft.com/cms/s/2/6da9f5bc-f08d-11e3-8f3d-00144feabdc0.html#axzz34kzPdWXd
[14] Health and Social Care Act 2012 http://www.legislation.gov.uk/ukpga/2012/7/section/1
[15] Yes Minister – “The Compassionate Society” (se2 ep1)
Created by Antony Jay & Jonathan Lynn. Broadcast February 23, 1981 – http://www.youtube.com/watch?v=x-5zEb1oS9A