The Partridge Review came out on Tuesday 17th and everyone should read it. But not just the summary. Both the full version and [1] summary are here.
The Partridge Review came out on Tuesday 17th and everyone should read it. But not just the summary. Both the full version and [1] summary are here.
So what is positive about these massive revelations? At long last it appears that the hands have come off the ears and the real issues are being listened to.
My summary: “NHS England cannot now put a hand over its eyes & hope care.data issues are only about communications.”
I feel somewhat relieved that the issues many have been concerned about for the last ten months, have now been officially recognised.
Amongst them, it has confirmed the utter lack of clear, publicly transparent and some quite basic, governance procedures.
It’s no surprise then, that our medical records, on at least two occasions in this sample 10% review of the releases, have gone to undocumented destinations. (Let’s ignore the fact of the other 90%!? of which we have no visibility yet).
At least eight insurers or re-insurers were in this 10% sample, so how many times did such companies get it, in the other 90% which has not been reviewed and we haven’t heard about?
How will ‘promotion of health’ purposes exclude them in future? In my opinion, it won’t.
Why would an insurance company be excluded if it requests data in order to provide health care coverage?
This is the wording of the Act, not ‘for the benefits of the NHS’ or any other more ‘friendly’ patient facing framing.
 At the NHS Open Day on Tuesday, the same day as the release, a panel spokesperson stated that commercial information intermediaries [2] will continue to be approved recipients. Gah – why this is such a bad idea, I wrote about here. [3]
At the NHS Open Day on Tuesday, the same day as the release, a panel spokesperson stated that commercial information intermediaries [2] will continue to be approved recipients. Gah – why this is such a bad idea, I wrote about here. [3]
The Partridge review said there had been no complaints. [4] MedConfidential pointed out an example of those of which they know. Kingsley Manning told the Health Select Committee [5] on 8th April, there had been seventeen opt outs of Hospital Episode Statistics, ever. Fourteen in 2013 and three prior to 2013.
“Q377Chair: There is not an opt-out rate for care.data yet, presumably.
Kingsley Manning: No, not on that, but in terms of the number of people who have acted to opt out, it is 3 opt-outs up until April 2013 and a further 14 opt outs since 1 April 2013.”
Would I be wrong to suspect each was accompanied by a complaint? You don’t usually opt out of something you are happy with.
The reason for these low numbers of both complaints and opt out in the wider public? WE DID NOT KNOW. The public didn’t know we had anything to be unhappy about. Many still do not.
As soon as I fully understood the commercial selling of my family’s patient records, this below is the query for advice / complaint I made in January to ICO, before the launch was postponed.
I wanted some guidance from an outside body, because I was being told the law permitted this extraction, so what good would a further complaint to HSCIC do? I had already written to my MP and had a response from the Secretary of State / Department of Health (which tried to tell me patient identifiable data was not shared with third parties), as well as feedback to my concerns raised by email with HSCIC, all of which only tried to reassure me. I had no one to otherwise raise concerns with. The ICO advisor I spoke to told me at that time, that they had had many similar complaints.
I’ll be blunt and say now, especially since the Open Day [more on that later, especially on the content of care.data FAQs we received], I think it’s fair to say I am far better informed about care.data than most in the public. When Mr. Kelsey asked for a show of hands, how many had heard of care.data, all put their hands up. Bearing in mind the rooms were full of highly involved people, NHS England staff, CCG and PPG leaders, and few ‘ordinary patients’ like me, and the agenda contained a section on care.data, it’s unsurprising we had heard of it. When Mr.Kelsey asked, “how many of you understand what it is?” the response was around 50%. I’d dispute also, that all of those 50% truly do.
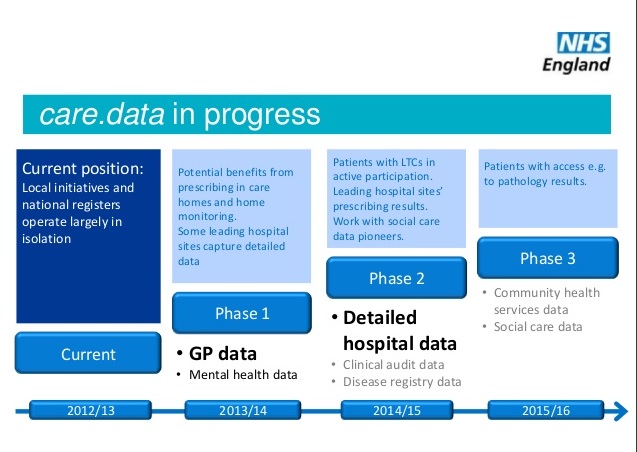
Some of the comms material we were given is factually incorrect, for example, around research. Currently, GP held data planned for care.data extraction and its merger with HES, into Care Episode Statistics (CES), is approved for commissioning purposes but not for research by the GPES group. It’s not approved for research purposes, so its no good telling us how good it is to have it for the benefit of research. What has already been released for research, and continues to be so, is what was already extracted in the past, with or without consent, and informing patients.
Records will not be deleted which raises all sorts of historical reporting concerns if mistakes are identified in retrosepct.
I have spoken with several NHSE Communications people who genuinely asked me, or left me asking the question for them in my own mind, “If I don’t understand it, then how is the public expected to?”
The concerns I had now almost five months ago, seem vindicated by the report. The actions taken since, the loose wording of the Care Act 2014, and little evidence of intention to make any change which is binding i.e. the opt out is only granted at the whim of the Secretary of State, it’s not statutory and that there is no independent governance to be put in place , have done nothing to bolster my confidence these gaps have been filled.
Simon Denegri, Chair of INVOLVE – the UK’s national advisory group on public involvement – and NIHR National Director for Public Participation and Engagement in Research, wrote a response on his blog [6]. I agree with the spirit of his post, and positivity, [he also writes excellent haiku] but where I disagree I outline below. There is room for positive hope for care.data, but first, let’s properly address the past.
“I am sure that many better informed people than I will pore over the detail. Others will use it to strengthen their case that we should put a stop to any manner of data sharing.”
Perhaps most key, I disagree with his fears the report could be used by ‘others.’ I don’t know anyone who wants to see a stop to ‘any manner’ of data sharing, including me. It’s the *how* and *why* and *with whom* that still needs work. Some of us may not want it without active consent, but that is part of the how, not if. It’s not *any* manner that I object to, it’s *this* manner specifically.
I have read the Review in detail and whilst there is much positive in attitude in the Review, the reality of what difference this will make with any real bite, is hard to find.
For example, “The HSCIC will plan a new ‘data laboratory’ service which will protect the public’s information by allowing access to it in a safe environment with HSCIC managed networks and facilities.” But this is with caveats, as it’s the “default,” Tim Kelsey said on Tuesday to the NHSE Open House. It does not mean *all* and if global third party intermediaries and business intelligence companies are still to receive data, then I can’t imagine the global likes of IMS Health, or Experian, or Harvey Walsh will send someone along to Leeds every time they want to extract data. Who will be given special permissions and how will they be decided and recorded, how will it be documented what data they access, if they get a free pass?
Unknown others have direct access to the HES system now through HDIS. Public Health should rightly use our health data, but a transparent list of all approved organisations here too, would be a positive step.
Simon’s post continues,
“As you would expect from a previous Chair of INVOLVE, Nick Partridge, has secured fundamental changes in the governance of HSCIC and data releases going forward. These include patients and the public sitting on the main committees reviewing data releases, open publication of data releases and a programme of ‘active communication’ with the public”.
Patients and public on the DAAG committee. If they are informed about data governance law and good practices, yes, if it’s just ‘representative’, not so useful. But DAAG is HSCIC staffed, and HSCIC has a legal and policy remit from the Department of Health and in its roadmap to distribute data, and will create ‘a vibrant market of data intermediaries’, as it would be wrong to exclude private companies simply on ideological grounds. So the concept of ‘independent’ is flawed. Where are the teeth needed to reject an application, if it’s in the interest of the reviewing body, to accept it?
“It’s my view that the Partridge review, its recommendations, and the swift response from the Health and Social Care Information Centre (HSCIC), offers us the opportunity of a fresh start with the public on this issue.” [S.D.]
This could be used as an opportunity to brush the past aside and say time for a fresh start, but it can only be so if there is confidence of change.
NHS England cannot now put a hand over its eyes and hope the issues go away or that it’s only about communications.
The past needs fisking, issue by issue, to avoid they happen again. And the real risks need addressed, not glossed over. Why?
Because let’s assume the public all thinks it’s fine, and none of us opt out. Then through these still flawed process holes, a huge data leak. The public loses trust all over again, and the opportunity for the care.data benefits is lost forever.
Get it right now, and you build a trustworthy and seaworthy future, for the future public good.
There are other more detailed questions I would raise, [I previously worked in functional database design amongst other things] and I will believe these recommendations will have an effect, if and when I see the words become actions. The Review by PwC and Sir Nick Partridge is a positive listening and speaking exercise, but the plans must become reality with actions, some under legislation, in my view.
And perhaps the simplest, unspoken point seems to being deliberately ignored as if just not seen, unmentioned, except by data protection gurus [7]. There is legal obligation to provide information to citizens before their data is released, in a transparent way, to whom and for what purpose. What happened to Fair Processing? [8] Past and present?
Sir Kingsley Manning, Chair of HSCIC, asked in the Guardian on 22nd January [9] that we have ‘intelligent, grown up debate’ about data sharing. Well my hand is certainly off my mouth. I wrote a feature in my local paper and I’m still speaking to anyone I can to promote fact-based informed decision making. But wider Public Debate is still sorely lacking [BBC Question Time anyone?] Through it, I’d like to encourage wider knowledge of the why, who and what of secondary purposes of data sharing and to ensure we can get it done transparently and safely.
Why?
To ensure we, as patients, continue to trust telling our GPs and hospital consultants all the information that we need to, and have no fear it will be held against us by an insurer or others.
We need to trust we will not be penalised whether through disclosure, by stigma and exclusion from policy or care; or whether by opting out, we could be penalised for not participating and not get ‘advantages’ offered to others, just like store loyalty cards.
We may think the insurance debate is irrelevant, if like me, we are not ‘self-payers’ or don’t use a private insurer. With a £30bn gap in planned budget and needed spend over the next five years, someone is still going to be paying for our healthcare.
If it’s not the State, then who? The risk more of us will pay for our own care in future is real. If not for us, for our kids, and their privacy will be a whole different ball game if genomics gets involved.
Meanwhile, we are told for care.data identifiable personal data is crucial for patient safety tracking. In my opinion, patient safety will be harmed if confidence in confidentiality fails. The relationship between clinician and patient will be harmed. And no number of Dr. Foster Intelligence reports by tracking quality or safety, will be able to fix those failures which it has helped create.
Perhaps most tellingly, NHS England is still to make a statement on the Review. There is no news yet here.
It still seems to me the NHS England leadership and its data sharing policy carried out through IC past and present, wants to continue without grown up debate under the PR motto ‘it’s all going jolly well’, and to act with the attitude of a teenager, who with a shrug of the shoulders will tell you:
‘It’s easier to ask for forgiveness than permission.’
***********
January 25th, 2014 – my ICO complaint / guidance request
{abbreviated only to show issues I feel still need addressed}
Dear ICO
I would like to ask for your urgent advice.
I am a mother of X children under 12. […] Our confidential patient data is being extracted via care.data to the HSCIC. Until my recent research to understand what this was all about, I did not know that HSCIC stored all our patient confidential health data from all sorts of health providers: Hospitals, Mental Health, National Child Measurement Programme, [10] Immunisations and Health visitors.
I have not knowingly given my permission for our data to be stored or transmitted to or from HSCIC in any format in the past. If by signing a consent form for treatment I also signed consent for sharing with this central body, it was without my knowledge and therefore without informed consent.
I have significant concerns over its use, now that I understand how widely our patient data may be used and now even shared abroad. [11] […]
There is no public information on :
1. How long our data will be stored for – data retention and data deletion and cross border governance
2. There is no opportunity for health record deletion of anything which was simply a mistake i.e.: recorded on the wrong record, or a misinformed opinion on lifestyle entered by the GP, not fact
3. How will future governance be assured that it will not be slackened to allow less strict pseudonymisation, and identifiable releases; for example to US firms who establish themselves in the NHS England healthcare market?
I do not believe that the legal rights created through the Health and Social Care Act are sufficient justification to overrule the Common Law of Confidentiality, and the Data Protection Act 1998. [And the data shared before 2012 was not covered by the Act which did not exist and was not retrospective.] Even if the dissent codes are applied, patient data has been or will be extracted to the HSCIC (without my permission) and it will contain identifiable items such as clinician name, practice and CCG locations, and referral dates which may be used as identifiers to connect with HES data stored at HSCIC – since HSCIC also holds data in the Personal Demographics Service [PDS], [12] I believe they may also link the data [13] then to my personal demographic identifiers. Just an undefined or internal governance procedure to suggest that they would not, when it is technically possible, is not sufficient oversight. […]
I do not consent for the use of our [hospital HES or other] data in health research – because it has not been explained to me, what that term means and the implications of this assumed consent.
I cannot know what the other future uses will be for our health information stored today. I do not feel that I can apply any fair processing to their health records due to the lack of publicly available information and scope of the full uses of their data today and in future. […]
Sincerely,
Jen Persson
XXXXXXX
———————————
[1] The Partridge Review Summary and Full report http://www.hscic.gov.uk/datareview
[2] On selling data to Intermediaries and the governance which permits it https://medconfidential.org/category/press-releases/
[3] Commercial users of NHS patient data – third party use – my blog https://jenpersson.com/flagship-care-data-2-commercial-practice/
[4] Complaints and why confidence needs restored https://medconfidential.org/2014/press-release-partridge-review-patients-need-proof-to-restore-confidence/
[5] Health Select Committee 8th April 2014 http://data.parliament.uk/writtenevidence/committeeevidence.svc/evidencedocument/health-committee/handling-of-nhs-patient-data/oral/8416.html
[6] Simon Denegri’s blog response to the Partridge Review http://simondenegri.com/2014/06/17/partridge-reviews-elegant-demolition-of-past-practice-on-personal-data-offers-opportunity-for-fresh-start-with-the-public/
[7] Information Rights and Wrongs – Jon Baines’ blog http://informationrightsandwrongs.com/2014/06/18/the-partridge-review-reveals-apparently-huge-data-protection-breaches/
[8] ICO Processing Data Fairly and Lawfully http://ico.org.uk/for_organisations/data_protection/the_guide/principle_1
[9] The Guardian, January 22nd 2014 ‘Lack of Debate on the Sale of Patient Information‘ http://www.theguardian.com/society/2014/jan/22/debate-sale-patient-information?CMP=twt_gu
[10] National Child Measurement Programme data managed by HSCIC http://www.hscic.gov.uk/ncmp
[11] Data use in the USA Memorandum between DH, HSCIC and the US Dept of Health and Human Services to include exploring secondary stores http://www.healthit.gov/sites/default/files/hhsnhs_mou_final_jan_21.pdf
[12] Personal Demographics Service http://systems.hscic.gov.uk/demographics/pds/contents data already stored at HSCIC
[13] Data Linkage Service at HSCIC to manage the requests for data which is stored in different silos and brought together on request http://www.hscic.gov.uk/dles
Image courtesy of an interesting post on the history of the featured monkeys: http://frontiersofzoology.blogspot.co.uk/2013/04/why-are-three-wise-monkeys-usually-apes.html

![Building Public Trust in care.data datasharing [3]: three steps to begin to build trust](https://jenpersson.com/wp-content/uploads/2015/06/optout_ppt-672x372.jpg)
![smartphones: the single most important health treatment & diagnostic tool at our disposal [#NHSWDP 2]](https://jenpersson.com/wp-content/uploads/2015/03/IMG_4563-e1427130930127-672x372.jpg)