“The challenge is that if many users of data are intermediaries with re-use licences and even the HSCIC doesn’t know who all the end users are, how on earth can anyone judge how they will be for purposes of ‘improving NHS care’?”
Commercial and third party use is one of the most damaging aspects of the rollout which is wrecking the care.data programme.
I’ve cut my opinion on this care.data topic into two parts, theory and practice, to address the outcomes of the LMC conf of yesterday from a patient POV. From my lay perspective, the result of the debate and votes was partly due to the failure to shore up the policy theory around commercial uses to make any perceivable improvement to trust for the future. And partly based on proven failures in practice to protect our data in the past. Failures around commercial use of care.data in theory and practice.
The theme of making money, is a recurring topic for women in literature, and graced or should I say, grubbied our screens in recent weeks in the adaptation of Dame Daphne Du Maurier’s Jamaica Inn.
Mary Yellan, orphaned and without means, seeks the only family she has and lands among the smugglers and muddy marsh of the Cornish moors. It’s not only set against a backdrop of smuggling, but wrecking. The heroine struggles between moral conflict and practical necessity, whether to join in their activities, against her ethical principles. She gets used to it but ultimately can’t live with it.
Given that the real inn is in the middle of a very bleak moor, with no outlook except the rough shorn grass, you need to really see unmet potential to want to be its new owner. For that, you need to see strong commercial opportunities or be a committed hard core Du Maurier fan. Or both.
So it can appear, from a patient point of view on care.data. Either the driving parties promoting the release of patient data see unmet potential [1] which needs commercial harnessing [1b], have direct commercial interests[1c], or they have another personal interest in its extraction and access. Or perhaps they are just hard core fans of data sharing, to the point that we should support mashing our health data up with commercial retail loyalty cards as Mr. Tim Kelsey suggested in November 2013 at Strata [from 16:00] [2].
Are the same people and organisations driving the programme and calling for ‘data for patients’ not also the same who will benefit most from having access to the data? The measurable benefits to us patients remain unclear, at best. The cost, our confidentiality and GP trust, is however clearly non-refundable. Consent, the age old pillar of medical ethics is to be waived aside. The LMC Conf obviously see value in protecting confidentiality at source if it cannot be guaranteed by others, whether the HSCIC or the data users.
Who will all the end users of our data be? They remain somewhat undefined, because the care.data addendum including Think Tanks, commercial companies and information intermediaries was not approved [3] and because future users are undefined in social care, for example. Future scope will entail additional future users. But then perhaps this should not surprise us that NHS England and the HSCIC expect us to acquiesce to this fair processing failure although we don’t yet know all the future end users, because Sir Kingsley Manning admitted that HSCIC does not know who all the current end users are either (Q272) [4a] at the Health Select Committee hearing. So, were the GPs at LMC Conf just expected to trust ‘on spec’ to whom their approval of care.data would entitle its sharing?
Information intermediaries in particular, seem to still be on the key stakeholders list[5] in January 2014. But only a year ago, in April 2013, The ‘Health and Social Care Transparency Panel’ discussion on sharing patient data with information intermediaries clearly stated there was no legitimate or statutory basis to share at least ONS data with them. [6]
“The issues of finding a legitimate basis for sharing ONS death data with information intermediaries for commercial purposes had been a long running problem. A number of possible approaches had been considered but advice from the relevant Government legal teams was that there did not appear to be a statutory basis for doing so. The panel identified this as a significant barrier to developing a vibrant market of information intermediaries (IIs). It also limited the ability of IIs to support NHS organisations with business intelligence to evaluate and benchmark the quality of their services.
It was agreed that this issue needed to be resolved, and if necessary changes to the relevant legislation should be considered. ”
I would love to know whether the law changed in the last year, how was the issue resolved, or has HSCIC and have we just through use, acknowledged that this sharing with intermediaries is acceptable and legal? The meeting later in July should have given clarity, but I can’t see minutes beyond April. They are no doubt somewhere, and someone cleverer than me, can help find them and clarify how the decision was reached I expect. I did find notes in the recent HSCIC audit of past data releases [4b], that ONS data was granted under existing law after all:
“The ONS data are supplied under the Statistics and Registration Service Act 2007 section 42(4) as amended by s287 of the Health and Social Care Act 2012, for the purpose of assisting the Secretary of State for Health, or the Welsh Ministers, in the performance of his, or their functions in relation to the health service.”
Since the Health and Social Care Act revoked the Secretary of State’s duty of care to provide a national health service, I wonder what functions it relates to as pertains to third party intermediaries? The ONS application form is detailed but no more enlightening for commercial intermediary use. I can’t help feeling we’re seeking justifications rather than good cause as the starting point for widening data releases. That we are starting to accept that our hospital records have been shared without our consent and sold. (Let’s give up the recouping costs word play, call a spade a spade. Data and cash change hands.). ‘What can we do about it anyway? we may well ask. As time has gone on in the care.data debacle, and in the three months since the delay, it appears from the leadership comments of NHS England from Mr. Kelsey in Pulse that, we’re not to worry, “now we are working to make care.data safe.” [free registration required] Still no one has said, we made a mistake of its handling in the past.
This acknowledgement however that work needs done to make the data safe, underlines exactly what so many saw months ago including the GPES advisory group which had concerns [17] in Sept 2013 on commercial uses and its communication, governance and patient trust. Care.data was launched regardless. Now it’s grounded. What has improved since then? What remains to fix?
How well exactly did HES storage and sharing work so far, with breaches identified as well as the basic legal fair processing failing to inform us of its extraction? What has been done to prevent it happening again? I have seen no concrete steps which give me faith the past flaws have been fixed enough to now trust it in future.
In February, before the pause Jeremy Taylor of National Voices wrote a very sound 12 point plan of what needed to change. Since then, what has actually changed [7] as far as I can see, is only the introduction of a delay, and that his words were listened to, that there should be no artificial deadline:
‘”the timescale for launching Care.Data was entirely artificial, as is the six month “pause”.
Three months into the delay, nothing of substance other than agreeing there is no artificial deadline, appears to have changed.
The most significant past let downs have all been commercial or third party uses. OmegaSolver, Beacon Dodsworth, PA Consulting, Earthware.
The Care Bill amendment touted as a change in the legal protection of our care.data, does not block commercial  uses of our data, only stating that it should be used ‘for the promotion of health’ which is open to all sorts of interpretation. Not least I imagine, those similar to ‘fight against obesity’ campaigns by marketing masters of commercialism.
uses of our data, only stating that it should be used ‘for the promotion of health’ which is open to all sorts of interpretation. Not least I imagine, those similar to ‘fight against obesity’ campaigns by marketing masters of commercialism.
So with little transparent change on policy, since we have become aware of data breaches, misuse and patient anger about commercial use, it should come therefore as no surprise that the BMA Local Medical Committees (LMCs) yesterday voted to state a preference for opt in not opt out, pseudo or anonymisation at source and insists that care.data should only be used for its stated purpose of improving health care delivery, and not sold for profit.
Simply: the public don’t trust that our identifiable data is protected and we object to all our data being traded commercially.
This is in direct conflict with HSCICs stated purpose in the HSCIC 2013-15 roadmap [8]:
“Help stimulate the market through dynamic relationships with commercial organisations, especially those who expect to use its data and outputs to design new information-based services.”
And in statements by both Sir Manning at the Health Select Committee and Dr. Geraint Lewis [9]:
…”we think it would be wrong to exclude private companies simply on ideological grounds; instead, the test should be how the company wants to use the data to improve NHS care. And, as Polly Toynbee put it, if “it aids economic growth too, that’s to the good.”
The challenge is that if many users of data are intermediaries with re-use licences and we don’t even know who all the end users are, how on earth can the HSCIC judge how they will benefit ‘improving NHS care’?
As regards economic growth, if the aim is to give away data for free, as Mr. Kelsey told the September 13th NHS England board (from 26:10)[10], how is the NHS to make profit from it? It’s not. Commercial companies are to buy at prices only to help HSCIC recoup costs [11], so that is not technically opposed in wording to ‘ not making a profit.’ Citizens, GPs and others can be aligned with that on paper. But not in spirit. For now commercial companies profit from our state funded records, paid for by NHS DoH money. They profit intermediaries with re-use licences beyond which we have no visibility or control of where our data goes or why. And the fact that the wider profiting third parties from the whole scheme, ATOS paid zero tax in the UK in 2012,[12] really grates. How does the cash given to ATOS benefit economic growth in the country?
Therefore, for the LMCs to have voted now any differently, would have expected them be soothsayers, knowing that the care.data work-in-progress and any future changes will make both the future scope purposes and future users clearly defined, in order to fulfil their duty as data controller, ensuring patients have a reasonable expectation of how their data will be used. It asks GPs to betray their age old fundamental principle of medicine, to betray patient confidentiality, for commissioning. They are being told to betray the good ethics of consent. They are being asked to betray patients’ trust and even to use that trust to ‘sell’ the idea in which they may not believe.
And care.data current processes betray the best practices of data collection – seek to collect the minimum data required, for a specific purpose and delete it when that is completed.
“Personal data processed for any purpose or purposes shall not be kept for longer than is necessary for that purpose or those purposes’ consistent with the Data Protection Act principle 5. [13]
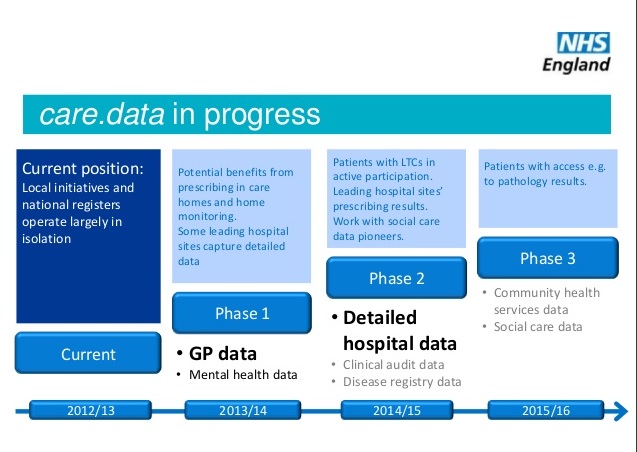
Instead HSCIC’s remit over the coming years of care.data is to fill in all the remaining gaps with any health and social care information not already collected [14], and keep it linkable from cradle to grave – or even from “germ to worm” for everyone with an NHS number in England. Purposes are non-specific and unlimited because they’ll change over time and the end users are not all defined for it plans to be opened up increasingly widely for use in social care and we don’t know what else.
In my lay view, the BMA LCs had no choice in the interests of their patients but to call for a rejection of assumed consent and commercial uses. The two do not go together. Opt out for uses of our data purely for NHS care and its planning would be much more palatable. But add in commercial uses, which is what has both been the main source of patient objection and data breaches, and it’s a deal breaker.
They can’t stake their support and reputation on a best guess of what might be. They can only base their judgement on what they know now. And no one supports care.data exactly as she is right now, which is why it is postponed and work in progress. Shore up trust, governance and axe these commercial uses and perhaps an assumed consent would seem more palatable. For example, Cross border governance needs documented when the application form gives non UK options. Scope and users need defined to ensure proper fair processing to meet DPA ICO requirements [16]. But so far, nothing has visibly changed.
It’s no different from when Ben Goldacre was telling us public trust cannot be easily regained and it broke his heart [15]. I know why, there are expected benefits to public research amongst others to access primary care data more than they already have in CPRD or pseudonymous data in QResearch and others, but we need to act based on today’s approved uses for care.data, not what might be remain in an undefined future. Right now, we’ve seen no changes of substance since the delay was announced.
NHS England can’t therefore genuinely expect to see a shift in trust in citizens or GPs based on nothing more than lines in the sand.
I believe GPs at the LMC Conf took the best decisions they could with the programme in its current form, with knowledge of past problems and lack of future clarity over scope and users.
They voted for how they feel best protects, respects and empowers their patients.
If our current Data Controllers and guardians of confidentiality don’t stand up for patients to get the build of the infrastructure right before they agree to release our data to fill it, who will? The question will be whether the Secretary of State and NHS England will force their legal right of extraction through regardless, or will respect the medical profession’s representatives and the rights of citizens they care for?
There is an opportunity to fix things. The LMC Conf after all have no legal efficacy, they stated their opinion and stance which commands respect and attention. Flagship care.data is not washed up, yet. But it can’t sail without addressing governance and professional support. Commercial exploitation and assumed opt in are not going to work comfortably together. Transparency of who has access to what data for what purposes and how it is released needs sharpened up. And regardless of whether opt in ever comes onto the table or not, if care.data keeps her strongly commercial heading many, many more will jump ship to opt out. The damage of bias will be done, either way.
She needs some new directions, helmsmanship that we trust and sound repairs.
********
If you have missed the background to this saga, I’d recommend the Julia Powles article in WIRED – what to save when the care.data ship goes down.
I’m going to look at some more of the commercial uses of care.data in practice another time. And clarify the communication of the opt out codes and why research purposes is a misnomer in the GP patient record sharing part of care.data purposes – it’s not (yet at least) an approved use.
********
[1] MOU between AstraZeneca and the HSCIC, December 2012
[1b] ABPI Vision for harnessing Real World Data 2011
[1c] Hansard, Nov 2010 George Freeman ‘I know from my own experience that we are sitting on billions of pounds-worth of patient data. Let us think about how we can unlock the value of those data around the world.’
[2] Strata November 2013, Tim Kelsey keynote ‘mash it up with other data sources to get their local retailers to tell them about their purchasing habits so they can mash that up with their health data’
[3] care.data addendum Sept 2013
[4] Written Hansard of the Health Select Committee , 8th April
[4b] The HSCIC data release register issued on April 3rd 2013
[5] Oversight panel with input from Dame Fiona Caldicott, January 2014, with stakeholders’ list
[6] Health and Social Care Transparency Overview Panel April 2013
[7] National Voices – Jeremy Taylor, an excellent overview of 12 points which needed fixed from February 2014
[9] NHS England comments by Dr.Lewis on commercial principle
[10] September 13th 2013, care.data directions approved by the NHS England Board – care.data from 25:40 – 39:00 – note identifiable, not anonymous data is extracted and stored with the DLES at HSCIC, and GP objections to date on care.data opt-in seem not to have been respected in contrast to the claim ‘GPs make a decision’ from 31:00. There is to date, no communicated way to prevent HES data extraction and its sharing in pseudonymous form.
[11] The HSCIC Data Linkage price list
[12] The Independent, November 2013 Atos & G4 pay no corporation tax in 2012, National Audit Office stats via Adam Withnall, The Independent
[13] Data Protection Standards – retention, principle 5
[14] care.data programme overview April 2013
[15] the Guardian, 28th February 2014 – care.data is in chaos – Ben Goldacre
[16] Blog from the Information Commissioner’s Office on care.data Data Protection and Fair processing
[17]The GPES Advisory Group meeting minutes Sept 12th 2013
{updated 28th May – looks like past uses of our health data are now also under scrutiny by ICO which is investigating claims that insurers have accessed full medical records using subject access requests.}
By [email protected]