Consent to data sharing appears to be a new choice firmly available on the NHS England patient menu if patient ownership of our own records, is clearly acknowledged as ‘the operating principle legally’.
Simon Stevens, had just said in his keynote speech:
“..smartphones; […] the single most important health treatment and diagnostic tool at our disposal over the coming decade and beyond ” Simon Stevens, March 18 2015.
Tim Kelsey, Director Patients and Information, NHS England, then talked about consent in the Q&A:
“We now acknowledge the patient’s ownership of the record […] essentially, it’s always been implied, it’s still not absolutely explicit but it is the operating principle now legally for the NHS.
“So, let’s get back to consent and what it means for clinical professionals, because we are going to move to a place where people will make those decisions as they currently do with wearable devices, and other kinds of mobile, and we need to get to a point where people can plug their wearable device into their medical record, and essentially manage their data as they wish.
“It is essentially, their data.”
How this principle has been applied in the past, is being now, and how it may change matters, as it will affect many other areas.
Our personal health data is the business intelligence of the health industry’s future.
Some parts of that industry will say we don’t share enough data. Or don’t use it in the right way. For wearables designed as medical devices, it will be vital to do so.
But before some launch into polemics on the rights and wrongs of blanket ‘data sharing’ we should be careful what types of data we mean, and for what purposes it is extracted.It matters when discussing consent and sharing.
We should be clear to separate consent to data sharing for direct treatment from consent for secondary purposes other than care (although Mr Kelsey hinted at a conflation of the two in a later comment). The promised opt-out from sharing for secondary uses is pending legal change. At least that’s what we’ve been told.
Given that patient data from hospital and range of NHS health settings today, are used for secondary purposes without consent – despite the political acknowledgement that patients have an opt out – this sounded a bold new statement, and contrasted with his past stance.
Primary care data extraction for secondary uses, in the care.data programme, was not intended to be consensual. Will it become so?
Its plan so far has an assumed opt-in model, despite professional calls from some, such as at the the BMA ARM to move to an opt-in model, and the acknowledged risk of harm that it will do to patient trust.
The NHS England Privacy Assessment said: ‘The extraction of personal confidential data from providers without consent carries the risk that patients may lose trust in the confidential nature of the health service.’
A year into the launch, Jan 2014, a national communications plan should have solved the need for fair processing, but another year on, March 2015, there is postcode lottery, pilot approach.
If in principle, datasharing is to be decided by consensual active choice, as it “is the operating principle now legally for the NHS” then why not now, for care.data, and for all?
When will the promised choice be enacted to withhold data from secondary uses and sharing with third parties beyond the HSCIC?
“we are going to move to a place where people will make those decisions as they currently do with wearable devices” [Widening digital participation, at the King’s Fund March 2015]
So when will we see this ‘move’ and what will it mean?
Why plan to continue to extract more data under the ‘old’ assumption principle, if ownership of data is now with the individual?
And who is to make the move first – NHS patients or NHS patriarchy – if patients use wearables before the NHS is geared up to them?
Looking back or forward thinking?
Last year’s programme has become outdated not only in principle, but digital best practice if top down dictatorship is out, and the individual is now to “manage their data as they wish.”
This shift in data creation, sharing and acknowledged ownership may mean epic change for expectations and access.
It will mean that people’s choice around data sharing; from patients and healthy controls, need considered early on in research & projects. Engagement, communication and involvement will be all about trust.
For the ‘worried well’, wearables could ‘provide digital “nudges” that will empower us to live healthier and better lives‘ or perhaps not.
What understanding have we yet, of the big picture of what this may mean and where apps fit into the wider digital NHS application and beyond?
Patients right to choose
The rights to information and decision making responsibility is shifting towards the patient in other applied areas of care.
But what data will patients truly choose to apply and what to share, manipulate or delete? Who will use wearables and who will not, and how will that affect the access to and delivery of care?
What data will citizens choose to share in future and how will it affect the decision making by their clinician, the NHS as an organisation, research, public health, the state, and the individual?
Selective deletion could change a clinical history and clinician’s view.
Selective accuracy in terms of false measurements [think diabetes], or in medication, could kill people quickly.
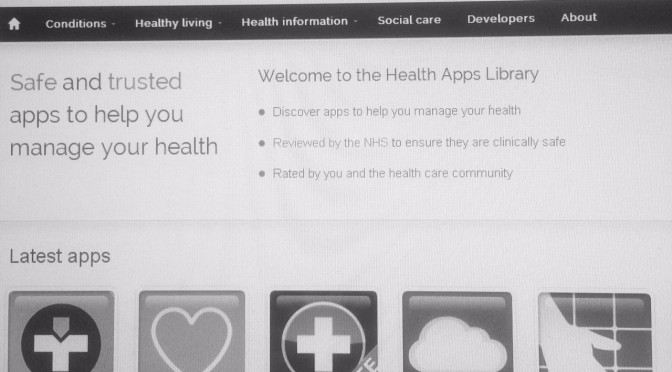
How are apps to be regulated? Will only NHS ‘approved’ apps be licensed for use in the NHS and made available to choose from and what happens to patients’ data who use a non-approved app?
How will any of their data be accessed and applied in primary care?
Knowledge is used to make choices and inform decisions. Individuals make choices about their own lives, clinicians make decisions for and with their patients in their service provision, organisations make choices about their business model which may include where to profit.
Our personal health data is the business intelligence of the health industry’s future.
Who holds the balance of power in that future delivery model for healthcare in England, is going to be an ongoing debate of epic proportions but it will likely change in drips rather than a flood.
It has already begun. Lobbyists and companies who want access to data are apparently asking for significant changes to be made in the access to micro data held at the ONS. EU laws are changing.
The players who hold data, will hold knowledge, will hold power.
If the NHS were a monopoly board game, data intermediaries would be some of the wealthiest sites, but the value they create from publicly funded NHS data, should belong in the community chest.
If consent is to be with the individual for all purposes other than direct care, then all data sharing bodies and users had best set their expectations accordingly. Patients will need to make wise decisions, for themselves and in the public interest.
Projects for research and sharing must design trust and security into plans from the start or risk failure through lack of participants.
It’s enormously exciting. I suspect some apps will be rather well hyped and deflate quickly if not effective. Others might be truly useful. Others may kill us.
As twitter might say, what a time to be alive.
Digital opportunities for engaging citizens as far as apps and data sharing goes, is not only not about how the NHS will engage citizens, but how citizens will engage with what NHS offering.
“We are going to move to a place where people will make those decisions as they currently do with wearable devices, and other kinds of mobile, and we need to get to a point where people can plug their wearable device into their medical record, and essentially manage their data as they wish.”
“we have got some very significant challenges to explore in our minds, and we need to do, quite urgently from a legal and ethical perspective, around the advent of machine learning, and …artificial intelligence capable of handling data at a scale which we don’t currently do […] .“I happen to be the person responsible in the NHS for the 100K genomes programme[…]. We are on the edge of a new kind of medicine, where we can also look at the interaction of all your molecules, as they bounce around your DNA. […]“The point is, the principle is, it’s the patient’s data and they must make decisions about who uses it and what they mash it up with.”
“This has got to be central about what the redesign of care looks like, with a fundamental power shift actually, in the way in which services are produced and co-produced.”
That could affect everyone in the NHS, with or without a wearables revolution.
These are challenges the public is not yet discussing and we’re already late to the party.
We’re all invited. What will you be wearing?
********
[Previous: part one here #NHSWDP 1 – From the event “Digital Participation and Health Literacy: Opportunities for engaging citizens” held at the King’s Fund, London, March 18, 2015]
[Previous: part two #NHSWDP 2: Smartphones: the single most important health treatment & diagnostic tool at our disposal]
Apple ResearchKit: http://techcrunch.com/2015/03/09/apple-introduces-researchkit-turning-iphones-into-medical-diagnostic-devices/#lZOCiR:UwOp